
Initiatives
National Network of Perinatal Quality Collaboratives (2017 - 2022)
The National Network of Perinatal Quality Collaboratives (NNPQC) provides resources and expertise to nationwide state-based perinatal quality collaboratives (PQCs) with the goal of deepening and accelerating improvement efforts for maternal and infant health outcomes.
The mission of the NNPQC is to support the development and enhance the ability of state perinatal quality collaboratives to make measurable improvements in statewide maternal and infant healthcare and health outcomes.
Keep scrolling, or use these quick links, to learn more.
What is a PQC? | Driver Diagram | Success Stories | Virtual Community | Helpful Resources | Related Content | Request Technical Assistance

Status: Complete
September 2017 to September 2022
- Who: PQCs in 47 states. Thirteen states—Colorado, Delaware, Florida, Georgia, Illinois, Louisiana, Massachusetts, Minnesota, Mississippi, New Jersey, New York, Oregon and Wisconsin—will receive targeted technical assistance as they develop their collaboratives.
- Funder: This project is funded by the Centers for Disease Control and Prevention (CDC).
- Our Role: As the coordinating center, NICHQ will enhance the coordination and communication of PQCs across the nation, advise state PQCs that are in early stages of developing their collaboratives, and give technical assistance focused on quality improvement (QI) methods that improve health outcomes for mothers and newborns.
If you are interested in learning more about this project, email: [email protected]
What is a PQC?
Perinatal Quality Collaboratives (PQCs) are state or multi-state networks of multidisciplinary teams, working to improve outcomes for maternal and infant health. PQCs do that by advancing evidence-informed clinical practices and processes using quality improvement (QI) principles to address gaps in care. PCQs work with clinical teams, experts and stakeholders, including patients and families, to spread best practices, reduce variation and optimize resources to improve perinatal care and outcomes. The goal of PQCs is to achieve improvements in population-level outcomes in maternal and infant health.
PQCs current areas of focus include:
- Reduce preterm births
- Reduce severe pregnancy complications associated with high blood pressure and hemorrhage
- Improve identification of and care for infants with neonatal abstinence syndrome
- Reduce racial/ethnic and geographic disparities
- Reduce cesarean births among low-risk pregnant women
Map of PQCs
The information in the map below is collected and updated annually from PQCs to reflect the most current information. Click the map below for more details.
Driver Diagram
Project Aim
By September 2018, all 13 state-based PQC grantee teams will be fully engaged with a statewide population-level perinatal improvement project. At a minimum, the project will include:
- Identification of project AIM
- Development of a measurement strategy including identification of appropriate outcome and process measures
- At least one statewide meeting with key stakeholders and participating teams
- Demonstrated progress with planning for use of data for improvement including ongoing monthly data collection of outcome and process measures
Essential Elements of a functioning PQC that should be in place by this time include:
- Multidisciplinary advisory committee
- Clinical leaders
- Public health leaders
- Quality Improvement advisors
- Family representatives
- Organizational structure and communication systems
- Data management plan
Primary Driver 1: Engagement and Buy In
Specific Ideas to Test or Change Concepts
- Leadership
- Identify and engage key players, including leaders/champions, hospitals, support staff, stakeholders and partners (payers and malpractice insurers), clinical experts, and family partners/advisors
- Leaders develop plans and design, including focus (neo. maternal or both), mission and goals
- Clarify roles and responsibilities (develop job descriptions)
- Use collaborative to develop and build teamwork at participating organizations
- Use recruitment package and informational calls, invitations from opinion leaders to promote engagement and buy in
- Funding - seek and secure funding
Primary Driver 2: Launching Initiatives
Specific Ideas to Test or Change Concepts
- Topics Selection - Choose topic based on impact, interest feasibility, and resources
- Focus/Vision/Mission/Goals of PQC
- Initiative topic selection based primarily on value perceived by participants (as well as public health burden/population, impact of the issue, interest feasibility, and resources)
- Clinical expert availability
- Develop Driver Diagram based on evidence based practice recommendations and success of previous like efforts
- Plan learning methodology – BTS or other
- Document variation in outcomes and success elsewhere
- Leadership - Recruit expert panel/advisory group
- Recruitment and Engagement of Participants
- Engage partner organizations (see below for potential organizations) to expand reach of initiative
- Use recruitment packages, informational calls, invitations from opinion leaders
- Collaborative Learning - Identify learning model (BTS or other), including plans for shared learning and accountability
- Evaluation - Plan evaluation, dissemination, and sustainability plans early on
- Use PQC website/branding for resource sharing and recognition
Primary Driver 3: Data Collection and Measurement
Specific Ideas to Test or Change Concepts
- Identification of measures and strategy for collection and analysis to maximize learning and minimize burden, including outcome, process and balancing measures
- Plan how teams will access data e.g. partnership with Vital Statistics
- Implement data sharing approvals and agreements
- Monthly data collection/reporting by all teams
- Determine plan for data analysis & feedback
- Educate teams to implement IRB vs. DSA
- Test feedback system prior to launch if appropriate
Primary Driver 4: Quality Improvement Methods
Specific Ideas to Test or Change Concepts
- Identify common Quality Improvement model for hospital use (MFI, LEAN, 6 Sigma)
- Provide QI model education and implementation throughout initiative - Provide coaching in QI including driver diagrams, Aim statements, measures, change packages
- Provide tools and resources for teams
Primary Driver 5: Dissemination
Specific Ideas to Test or Change Concepts
- Develop Dissemination Plan
- Including specific publication plan
- Design from overview, dissemination goals, target audience, messages, channels
- Develop Communication Plan – Early and frequent communication from plan of action to results
Primary Driver 6: Sustainability
Specific Ideas to Test or Change Concepts
- Planning for sustainability- Design based on funding level (minimal, limited, moderate, and substantial)
- Supports and Resources- Plan supports for sustainability (stakeholders, partners, successes, marketing)
Success Stories
California
Led an initiative to launch a data center to track performance on maternity care service in real-time to support work to reduce severe maternal morbidity and non-medically indicated deliveries before 30 weeks gestation. It resulted in more than 100 hospitals actively submitting data, which provided benchmark statistics comparing hospital performance to county, system, regional and statewide statistics, as well as allowed for analysis at the patient and physician level to identify specific quality improvement opportunities. Read the full case study.
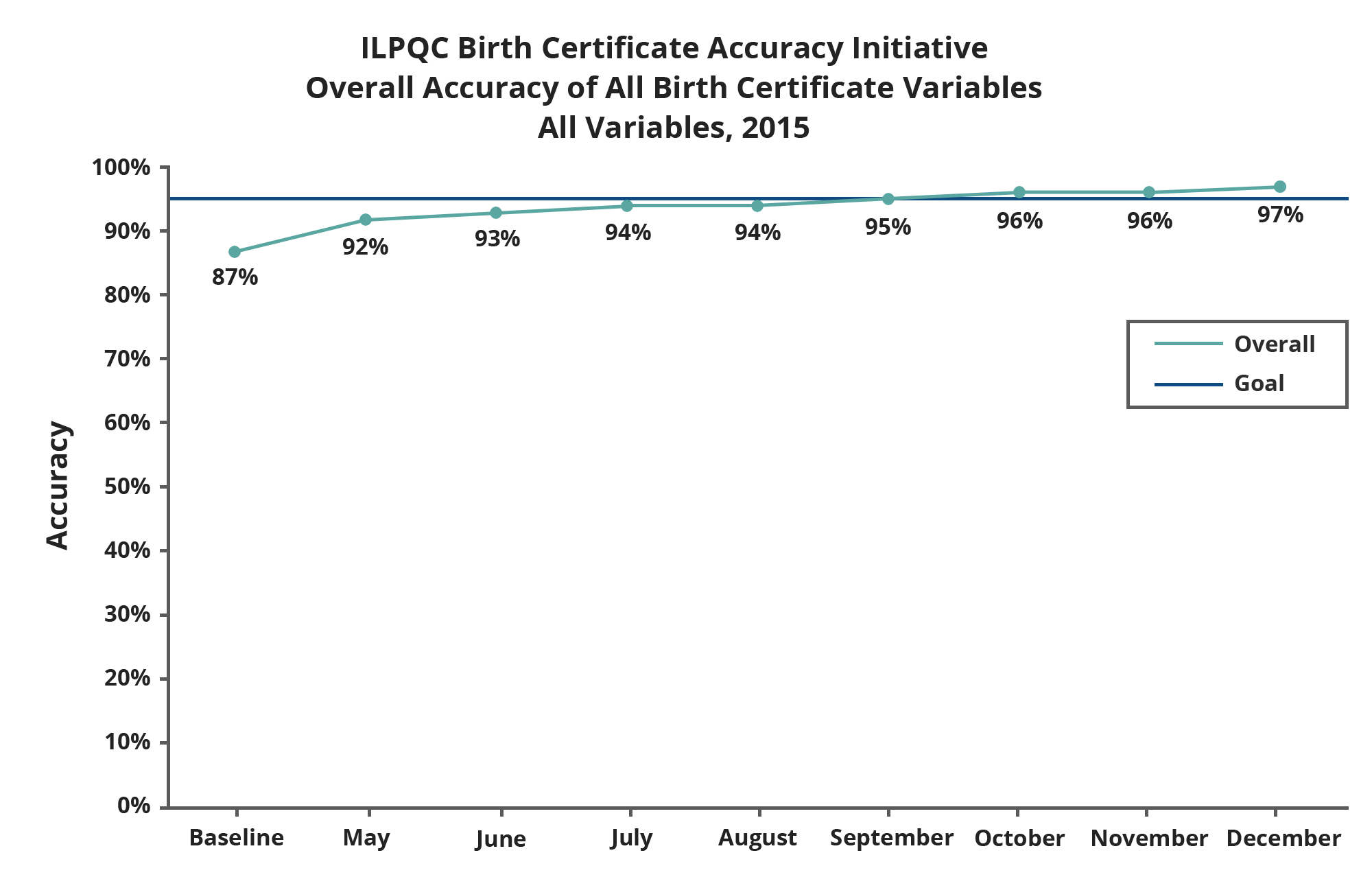
Illinois
Led an initiative to improve the accuracy of birth certificate data. It resulted in improved accuracy on all birth certificate variables from 87 percent at baseline to 97 percent at completion. Read the full case study.
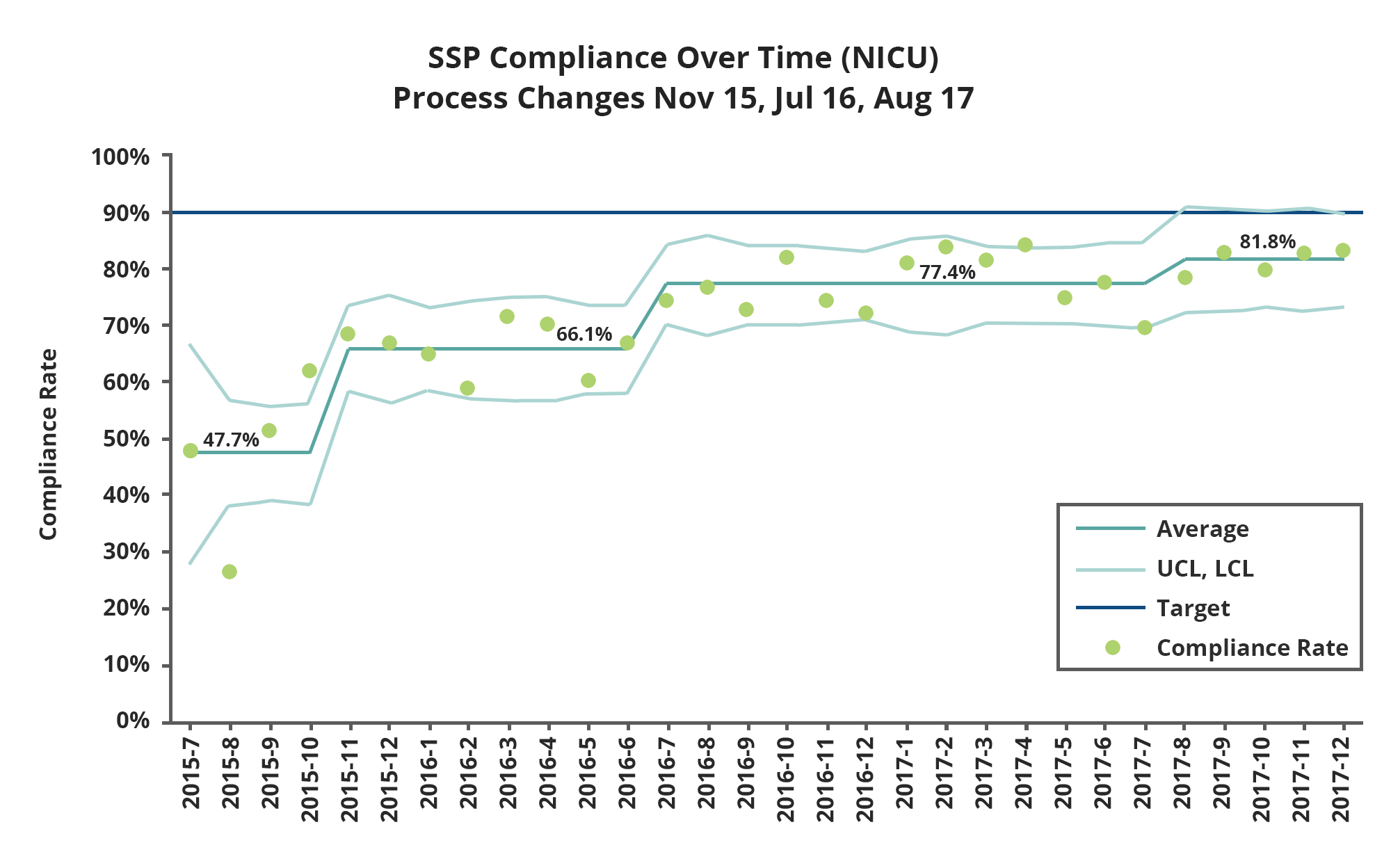
Massachusetts 1
Led a statewide initiative to implement safe sleep practices in all level III neonatal intensive care units. Among eligible infants, overall safe sleep compliance improved from 48 percent to 81 percent; variability across hospital sites was significantly improved, with compliance among hospitals ranging from 9 percent to 91 percent in 2015 and from 64 percent to 97 percent in 2017. This in-hospital quality improvement effort is now expanding to collect post-discharge data on adherence to safe sleep practices in the home. Read the full case study.
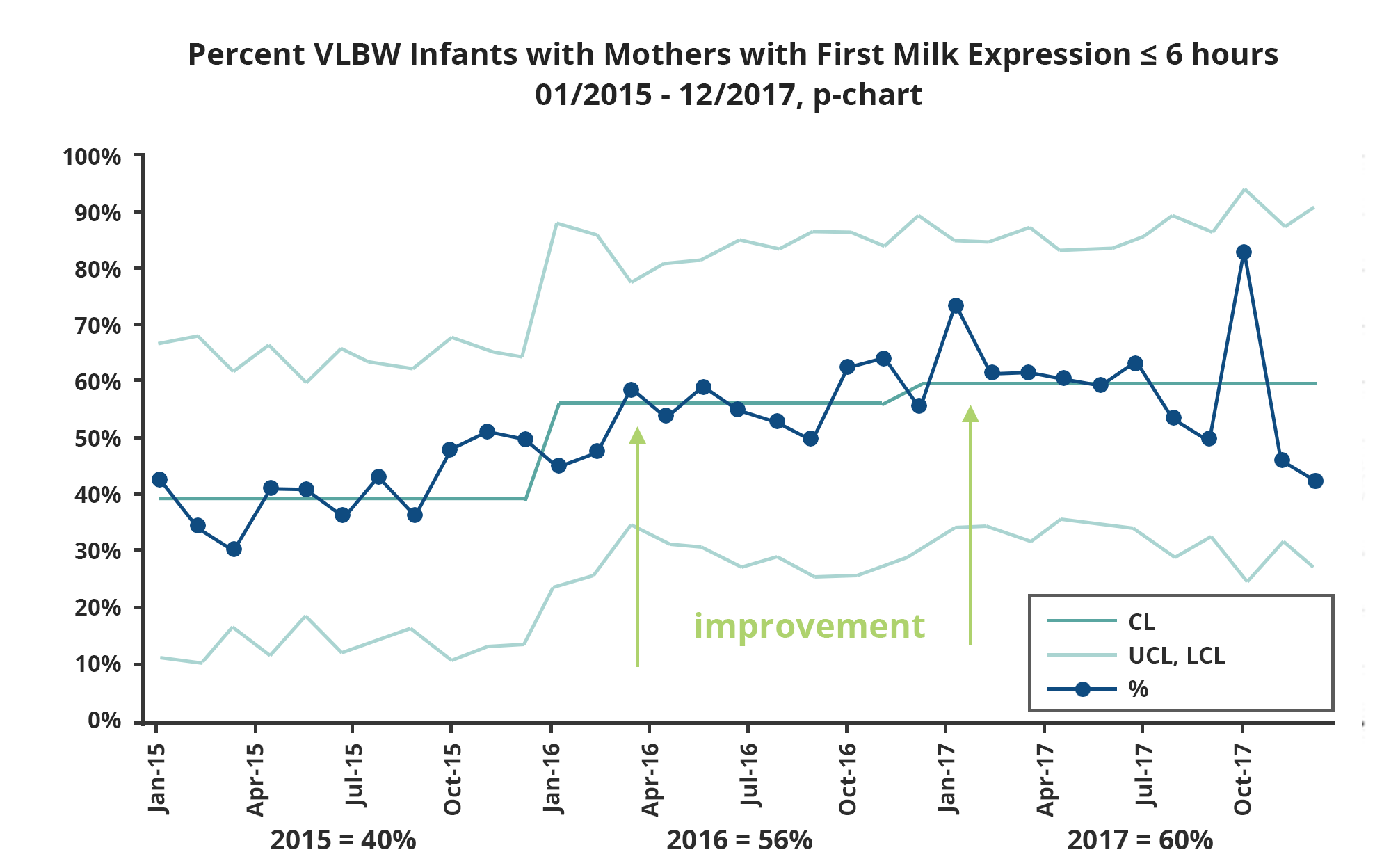
Massachusetts 2
Led a statewide initiative among all 10 level III neonatal intensive care units to improve mother's milk use for very low birth weight infants and to reduce racial/ethnic disparities in mother's milk use. Over the three-year collaborative from 2015 to 2017, prenatal consultations with human milk education increased from 60 percent to 82 percent and early milk expression within six hours after delivery increased from 40 percent to 60 percent. Overall, >80 percent of very low birth weight infants received mother's milk a one month and 63 percent at discharge. There was center-to-center variation in racial/ethnic disparities, but overall non-Hispanic whites had the highest rate of any mother's milk, followed by non-Hispanic blacks, followed by Hispanics. Read the full case study.
New York
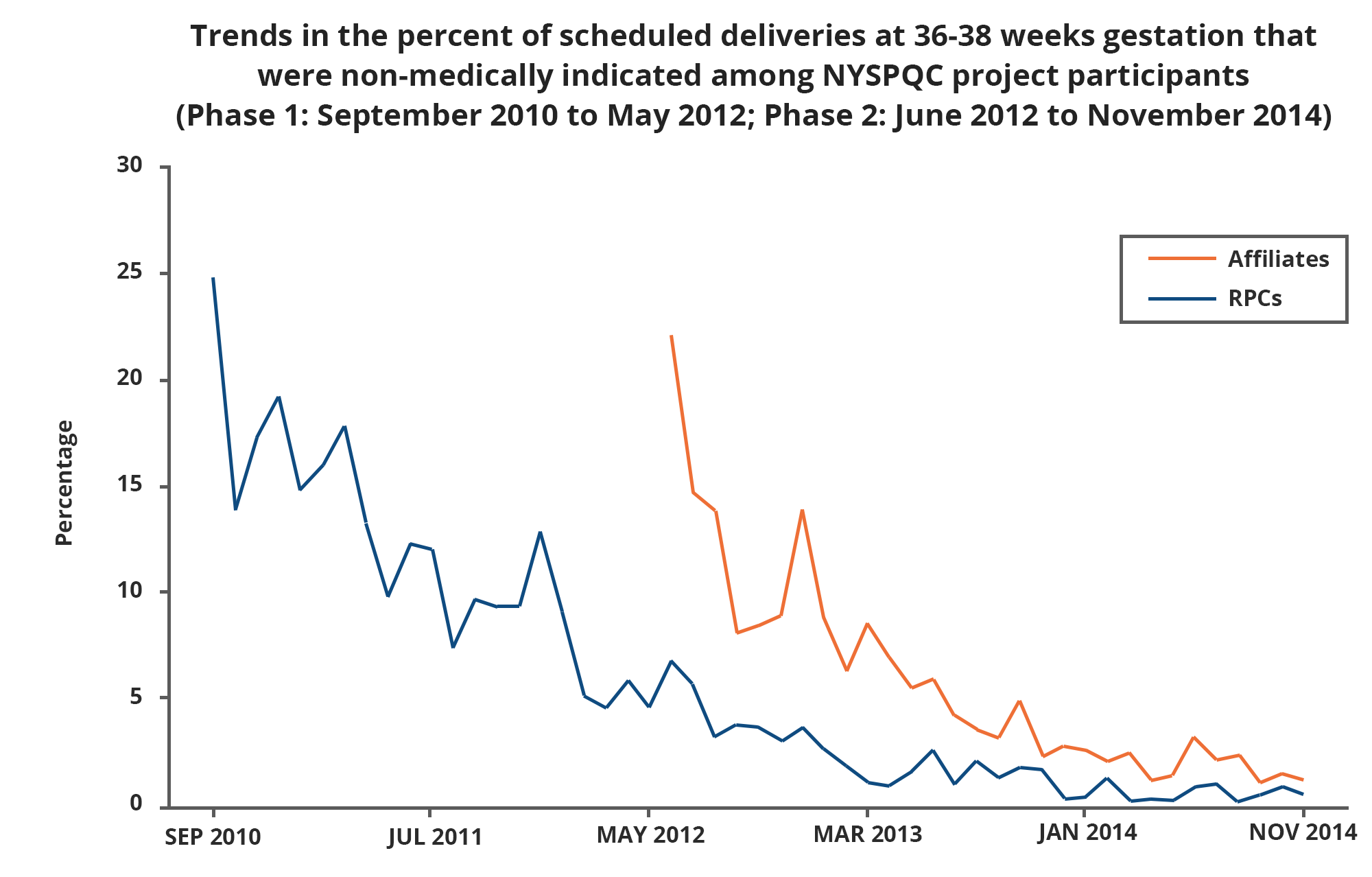
Led an initiative to reduce scheduled C-sections and inductions without a medical indication from 36 weeks up to 39 weeks gestation. As a result, Regional Perinatal Centers (RPCs) saw a 97 percent decline in scheduled deliveries without a medical indication between September 2010 and November 2014 and affiliates saw a 94 percent decline in scheduled deliveries without a medical indication between June 2012 and November 2014. Read the full case study.
North Carolina
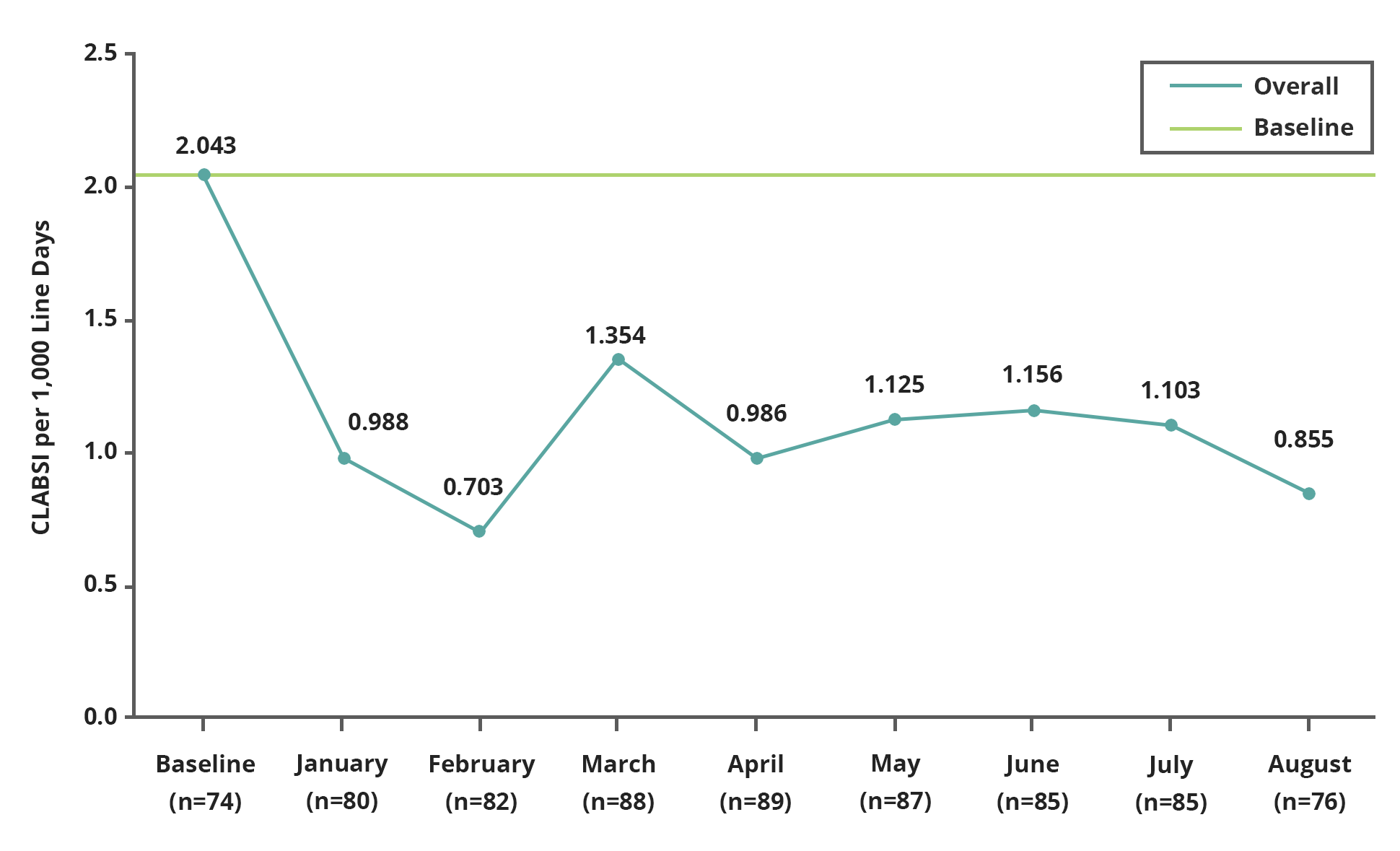
Led a national initiative to reduce central line-associated bloodstream infections (CLABSI) in neonatal intensive care units (NICUs). It resulted in an almost 60 percent decrease in CLABSI rates in 11 months. The project prevented an estimated 131 infections that translated to an estimated 14 to 41 deaths prevented, and over $2.2 million in excess costs avoided. Read the full case study.
Join Our Virtual Community
The NNPQC Collaboratory (CoLab) is a virtual place where NNPQC participants and stakeholders can share ideas and best practices, ask questions, and uncover useful tips to advance their change efforts. If you are a member of your state’s PQC, join CoLab and access the online Consultant’s Bureau to request technical assistance from experts in the field!
Already a member?
Want to join? Click the Log In link above and then click "Create a new account."
Helpful Resources
We've curated several resources for those working on early childhood health:
- CDC PQC Guide
This guide provides states with assistance as they form and develop their PQCs. - PQC Webinar Series
Learn about upcoming webinars hosted by the NNPQC that allow PQCs to share strategies related to their development as well as specific perinatal quality improvement initiatives. - Map of PQCs
Discover existing PQCs and contact information or PQC leads. - Quality Improvement 101 E-Course
This interactive course teaches the fundamentals of quality improvement and how to use this methodology to create effective, beneficial change. - Quality Improvement 102 E-Course
This interactive course reviews the concepts covered in QI 101 and then gives direction on how to test improvement ideas and increase their impact and effectiveness. - Essentials of Collaboration E-Course
This interactive course explores how to produce positive population health outcomes through effective collaboration. - Webinar recording: Opioid Use Disorder in Pregnancy and Neonatal Abstinence Syndrome
In this recorded webinar, experts discuss the benefits of universal screening for opioid use in the prenatal period and identify best practices of caring for a mother during the prenatal period.
Request Technical Assistance
Is your perinatal quality collaborative in need of technical assistance or support? Complete this form and a member of our team will contact you as soon as possible.
